Under normal circumstances, female vaginal microenvironment is affected by menstrual cycle, hormone level (including pregnancy status), diseases (diabetes, immunosuppressive diseases), antibiotic drug use, sexual partners and other factors. The pH value of the vaginal microenvironment is about 3.8-4.5. The main microorganisms commonly found in the vagina include Lactobacillus, Staphylococcus, Streptococcus, Escherichia coli, Candida, and Gardnerella vaginalis. According to existing literature, there is currently a general consensus on the protective role of lactobacilli in maintaining the vaginal microenvironment of women of childbearing age. An appropriate amount of lactobacilli can reduce the negative charge on the cell surface and remove the sugar groups covering the receptor surface by producing substances such as lactic acid and hydrogen peroxide, exposing the receptor and helping bacteria adhere to the antimicrobial factors produced in lactobacilli metabolism, thereby forming a physical protective barrier, inhibiting substances such as Escherichia coli and Candida to block the adhesion of normal vaginal epithelial cells, reducing the nutrient uptake of pathogenic bacteria, and inhibiting the proliferation of pathogenic bacteria. The underworld of the vagina is unfathomable. Although it doesn't speak much, it often becomes inflamed.
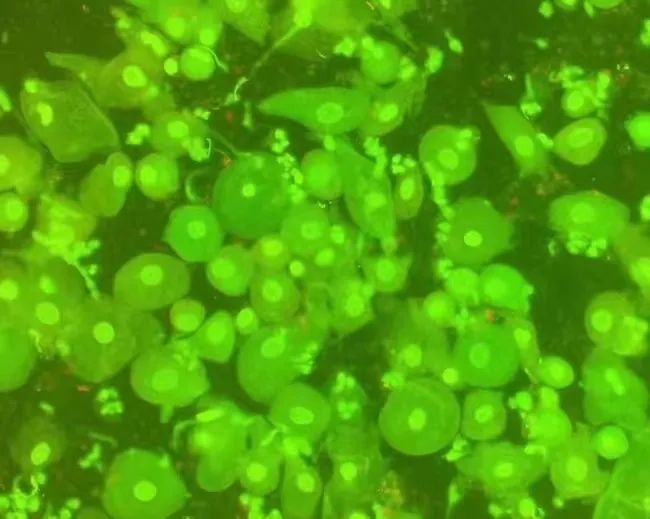
colpitis mycotica
Fungal vaginitis or candidal vaginitis, also known as vulvovaginal candidiasis (VVC), is a common and multiple vulvovaginal inflammatory disease caused by Candida.
Clinical manifestations:
The typical symptoms of candidal vaginitis are itching of the external genitalia, which can be mild, severe, and intermittent. Severe itching can lead to restlessness, difficulty sleeping and eating, and even painful urination and sexual intercourse when inflammation is severe. Increased vaginal discharge is another major symptom of this disease, which is usually thick and appears as bean dregs or milk clots. Fungal spores and hyphae can be detected in smears of vaginal secretions.
It is common for pregnant women to suffer from fungal vaginitis in clinical practice. This is because high estrogen levels during pregnancy lead to a high glycogen content in the vaginal environment, which provides abundant material conditions for the growth of Candida albicans (commonly known as mold). Therefore, pregnant women are prone to fungal vaginitis.
Treatment:
The treatment principle for vulvovaginal candidiasis during pregnancy is: the primary issue that must be considered during treatment is whether the medication is harmful to the fetus; The treatment mainly focuses on local medication and does not involve systemic medication; Only for pregnant women with symptoms and signs.
bacterial vaginitis
Bacterial vaginitis (BV) is a syndrome caused by a mixed infection of Gardnerella vaginalis and some anaerobic bacteria, leading to an imbalance in the vaginal microbiota, increased vaginal discharge, fishy odor in vaginal discharge, and itching and burning of the external genitalia.
Diagnosis:
1. Vaginal secretions are grayish white, viscous, like a paste, uniform and consistent, and non purulent.
2. The pH value in vaginal secretions increases from 5.0 to 5.5, while the normal range is from 3.8 to 4.5.
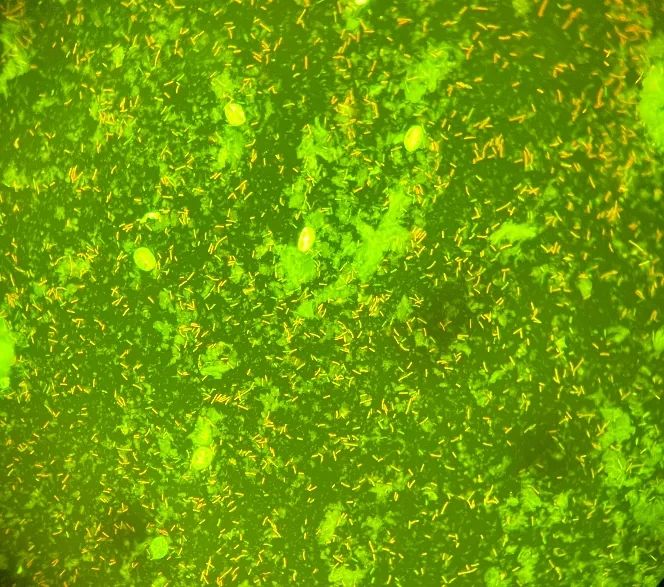
3. Clue cells can be detected in immunofluorescence smears of vaginal secretions.
Trichomonal vaginitis
Trichomonas vaginitis is one of the common vaginitis caused by trichomonas vaginalis infection, and its transmission routes mainly include two ways: first, direct transmission through sexual activity; The second is indirect transmission through public goods such as bathtubs, swimming pools, towels, foot basins, and toilets. Trichomonas vaginalis can cause trichomoniasis when it parasitizes the female vagina. Trichomoniasis vaginitis can be treated with external therapy.
Diagnosis:
The typical symptoms are itching, burning pain and sexual intercourse pain at the vaginal orifice and vulva. The leukorrhea increases in thin foam like, yellowish green, and has a foul smell. Trichomonas vaginalis can also invade the urethra or paraurethral glands, even the bladder and renal pelvis. If combined with urethral infection, there may be frequent urination, urgency, pain, and sometimes hematuria.
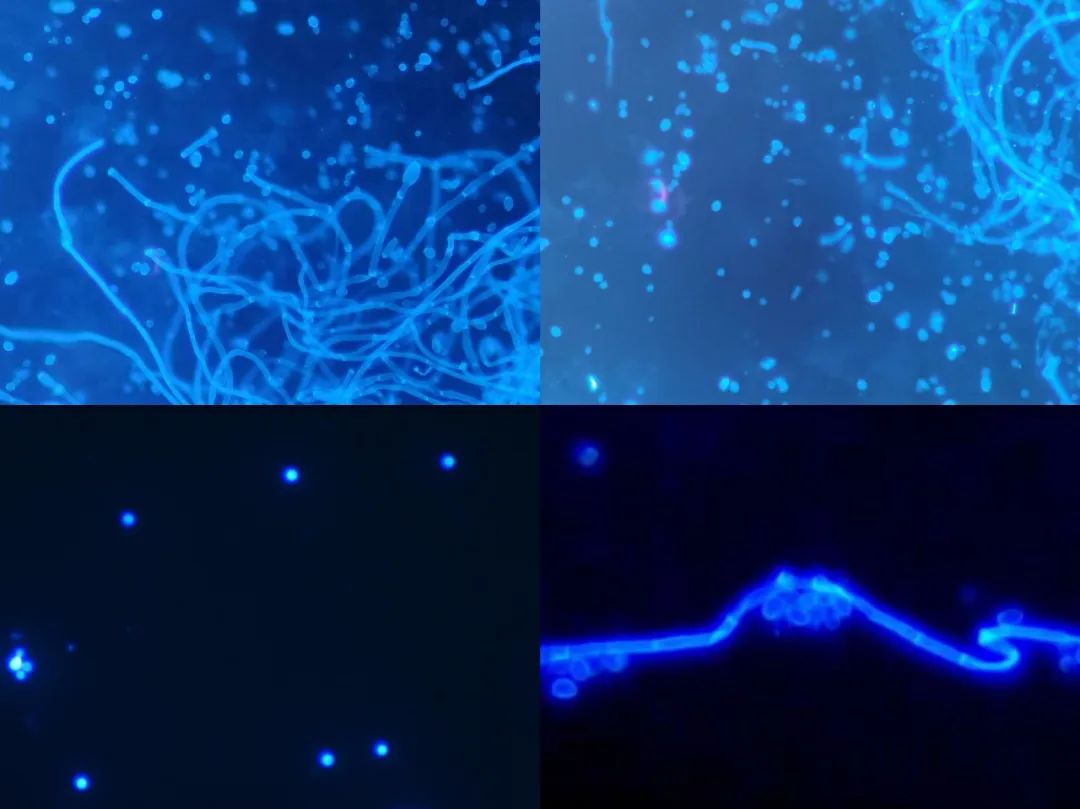
Immunofluorescence smear examination:
Just smear and examine the vaginal secretions taken from the posterior fornix under a microscope. It is easy to observe the rapid extension movement of flagella and the sprinting activity of ovoid protozoa. If the trichomonas have become inactive, inverted pear shaped or nearly circular trichomonas can be observed, and flagella can generally be observed.
Cytolytic vaginitis
Cellular lytic vaginitis is a disease mainly caused by excessive proliferation of lactobacilli and low pH, which leads to the dissolution and rupture of vaginal squamous epithelial cells and causes corresponding clinical symptoms. The common clinical manifestations of patients are itching of the external genitalia, burning discomfort of the vagina, and the nature of vaginal secretions is thick or thin white cheese like.
Common clinical manifestations may include vaginal discharge odor, itching, external genital/vaginal erythema or burning discomfort, and difficulty during sexual intercourse. The discharge often appears as white bean residue. The occurrence of CV is related to the secretion level of estrogen during the menstrual cycle, which worsens during the luteal phase; During menstruation, the flushing of menstrual blood causes an increase in vaginal pH, which alleviates symptoms.
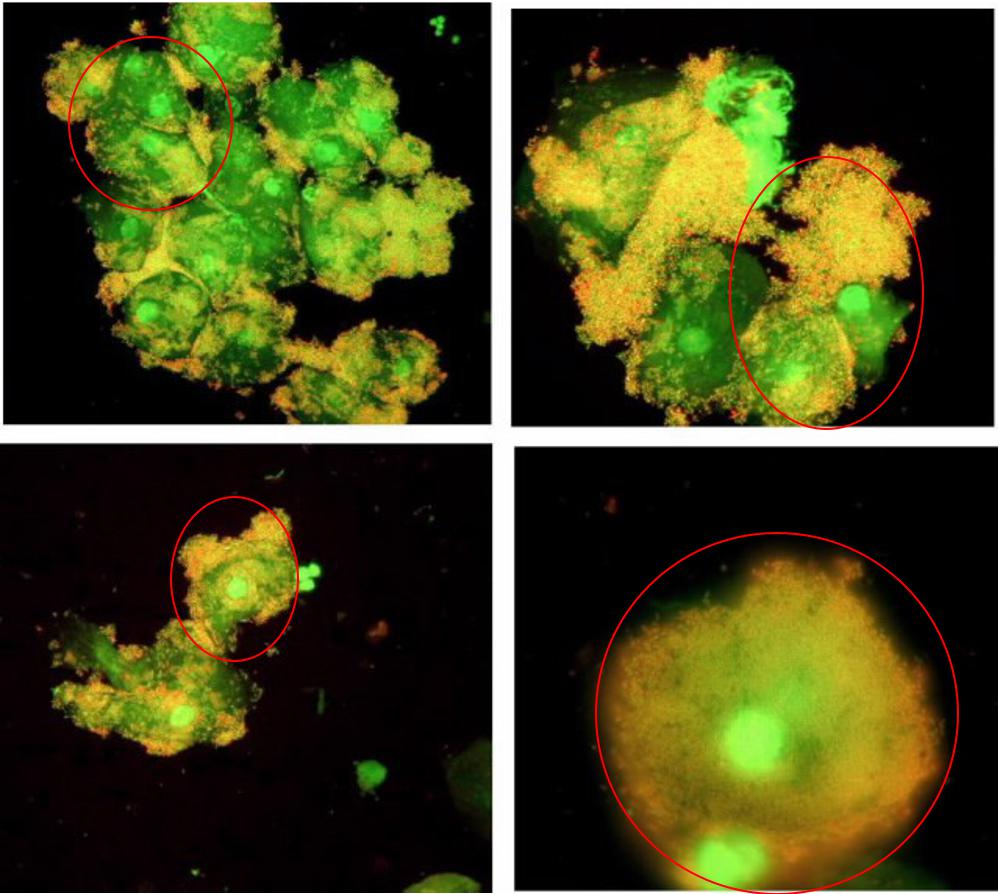
Immunofluorescence smear examination:
The vaginal pH value of patients with this disease is usually between 3.5 and 4.5, which is lower than that of the normal population. Immunofluorescence smear examination of vaginal secretions showed no fungal hyphae, spores, trichomonas, or Gardnerella genus, but a large number of large bacteria, fragmented cytoplasmic fragments, and naked nuclei of epithelial cells. White blood cells were rare or even absent.
The clinical symptoms of CV are very similar to vulvovaginal candidiasis (VVC), and are often overlooked or misdiagnosed as VVC or recurrent VVC in clinical practice, leading to incorrect treatment.
Treatment:
CV treatment is relatively simple, and the core is to correct the low vaginal pH value. The treatment plan mainly involves taking a sitz bath or vaginal rinse with 30-60 g of sodium bicarbonate and 1 L of warm water, twice a week, for a course of treatment.
Aerobic vaginitis
Aerobic vaginitis (AV) is a common clinical vaginitis caused by a decrease or absence of lactobacilli in the vagina and an increase in aerobic bacteria. The diversity of vaginal microbiota in AV patients increases, and the pathogens are relatively complex, with a common increase in various aerobic and facultative anaerobic bacteria such as Group B Streptococcus, Escherichia coli, Staphylococcus aureus, Enterococcus faecalis, Streptococcus pharyngitis, Klebsiella pneumoniae, etc. In addition to the complex characteristics of pathogens, AV is also prone to other vaginal infections.
Clinical symptoms:
10% to 20% of AV patients are asymptomatic. Symptoms mainly manifest as yellow vaginal discharge, odor, burning or stinging sensation in the external genitalia, and painful intercourse. Physical examination shows symptoms such as vaginal mucosal redness, swelling, ulcers, or a certain degree of vaginal mucosal atrophy. Symptomatic individuals have symptoms that persist for a long time, intermittently worsen, and are prone to recurrence after treatment.
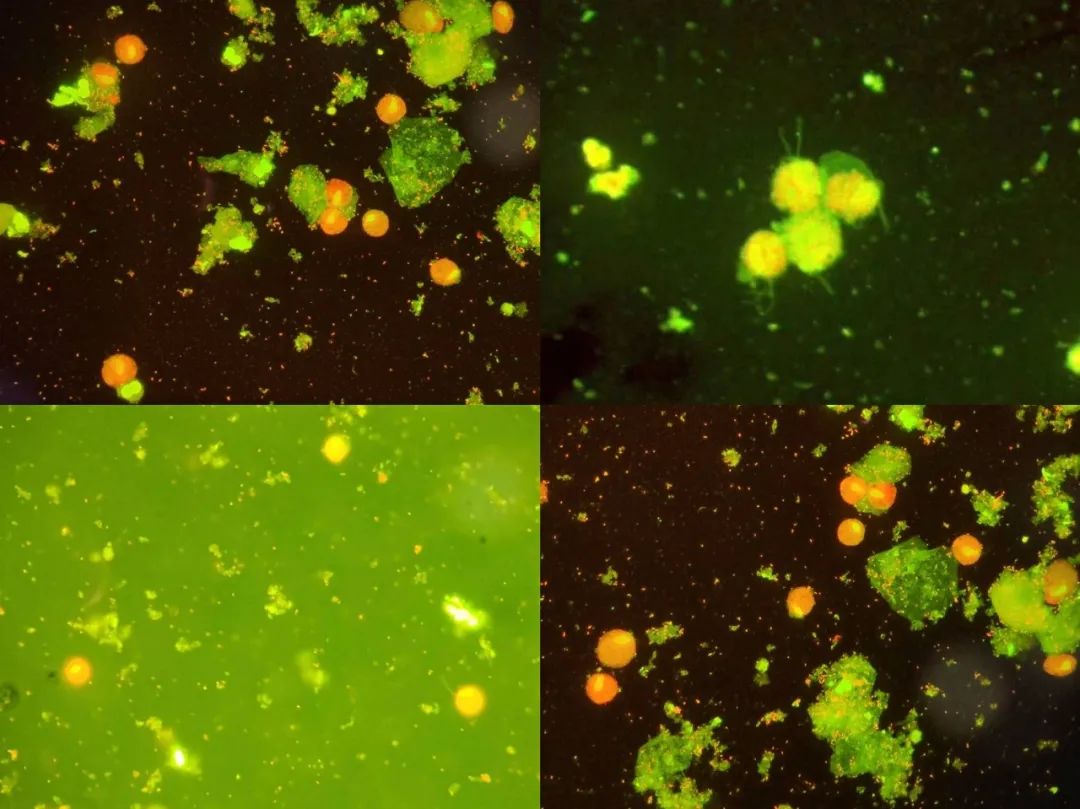
Diagnosis:
Immunofluorescence smear examination of vaginal secretions shows abnormal bacterial flora (non BV flora) and concurrent inflammatory response, with a large number of white blood cells visible under the microscope.

Treatment:
AV is often associated with mixed vaginal infections. Before treatment, a thorough evaluation should be conducted to determine the presence of other vaginal inflammations, such as bacterial vaginosis, trichomoniasis, and vulvovaginal candidiasis.
Targeted medication for determining the type of infection, combining traditional drugs with microbiota preparations, can prolong the recurrence interval of AV and restore normal vaginal microbiota. Male sexual partners of AV patients do not require routine screening and treatment. If the symptoms persist or recur, follow-up and re examination are required. Follow up vaginal microbiota testing after treatment to evaluate the recovery of vaginal flora and efficacy.
Exfoliative inflammatory vaginitis
Desquamatous inflammatory vaginitis (DIV) is a relatively rare and unexplained vaginitis characterized by persistent purulent vaginal discharge, vaginal erythema, and cervical vaginal submucosal bleeding. DIV usually presents with a chronic course, ranging from several months to several years or even more than ten years, and inflammatory response is the main characteristic of this disease.
The specific diagnosis can be summarized as follows:
1. Abnormal vaginal discharge or pain during sexual intercourse;
2. Vaginal pH value greater than 4.5;
3. Immunofluorescence smear examination shows that the ratio of white blood cells to vaginal epithelial cells is greater than 1, and the number of parabasal cells exceeds 10% of the total number of epithelial cells. The vaginal microbiota shows a decrease in bacteria, an increase in cocci, and wireless cord cells;
4. Normal ovarian function;
5. Vaginal antibiotic treatment quickly takes effect;
6. Exclude other diseases.
Immunofluorescence smear examination:
Immunofluorescence smear examination showed that the ratio of white blood cells to vaginal epithelial cells was greater than 1, and the number of parabasal cells exceeded 10% of the total number of epithelial cells. The vaginal microbiota showed a decrease in bacteria, an increase in cocci, and no cordless cells.
Immunofluorescence detection of gynecological vaginal discharge


